Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.
Christopher Malin had always been diligent about his health, so he was used to getting the basic tests — blood pressure readings and blood tests for cholesterol and glucose levels. The 59-year-old Melville, N.Y., resident knew he faced a higher risk of heart disease because of blood pressure that remained high despite medications and a family history of cardiac problems.
Malin thought he’d covered all the bases. But at a visit with his primary care doctor in early 2023, the grandfather of one mentioned a new development — dull, come-and-go pain in his left shoulder and arm when exercising. He soon found himself getting an electrocardiogram (EKG) to gauge his heart’s electrical activity and an exercise stress test with nuclear imaging. Those exams prompted a referral to Northwell Health cardiologist Jeffrey Kuvin, MD, who looked at Malin’s risk factors, symptoms and test results and quickly set up a coronary angiogram.
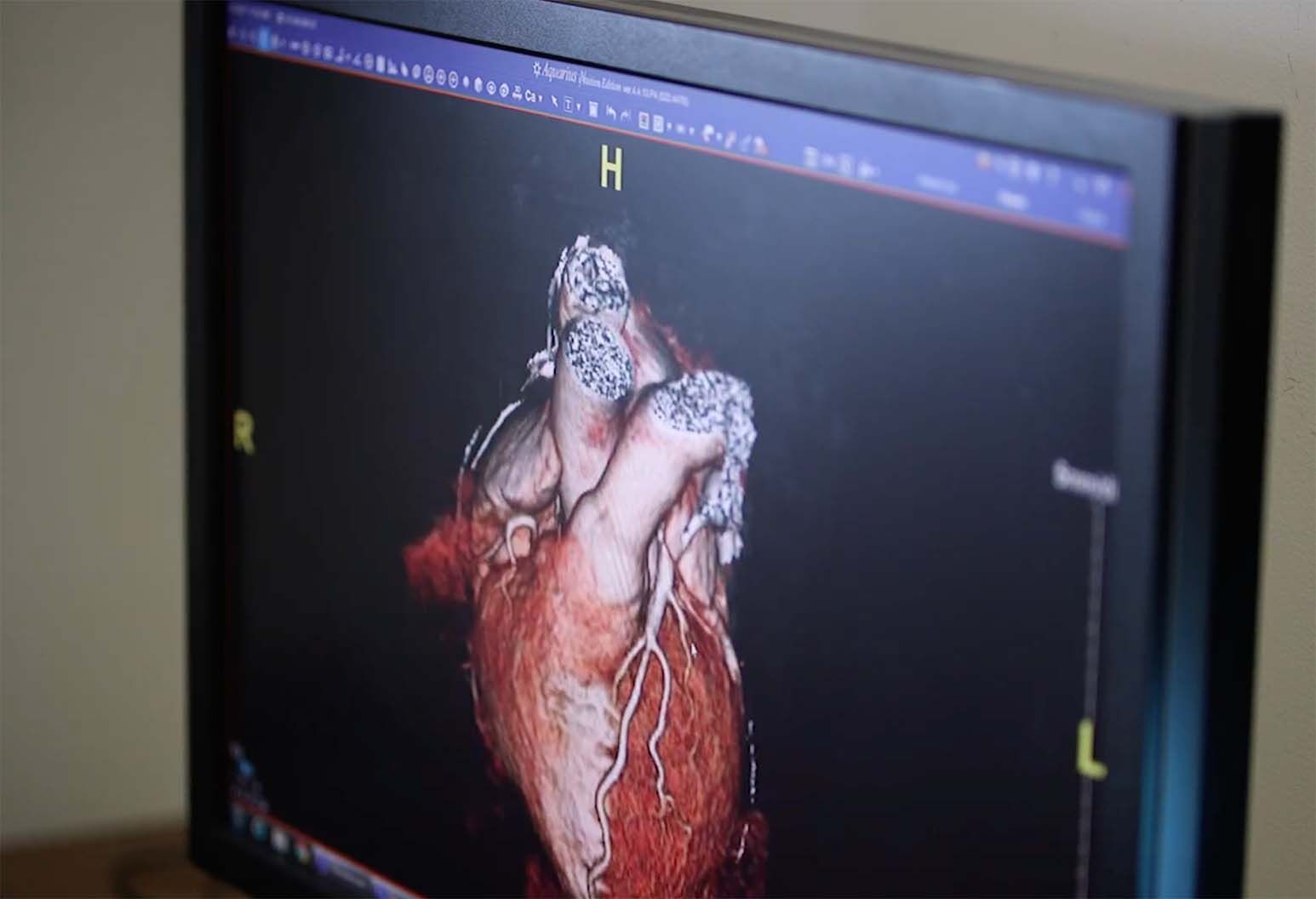
The results made the scope of Malin’s heart problem stunningly clear: He had a 99% blockage of his left anterior descending (LAD) artery. A heart attack originating in the LAD is sometimes called a “widowmaker” because the artery plays such a key role in supplying blood to the heart. The interventional cardiology team fixed the problem on the spot, inserting a mesh stent in Malin’s LAD to prop it open. Six hours later, Malin went home, healthy, grateful and ready to adopt the medications and lifestyle changes his doctors advised.
“I’ve got pictures of my heart that clearly show the before and the after,” says Malin. “It’s very alarming how close I was to a tragedy.”
“He was able to avoid a major — and perhaps life-ending — heart attack,” agrees Dr. Kuvin, senior vice president of cardiology at Northwell Health and co-director of the Sandra Atlas Bass Heart Hospital at North Shore University Hospital. “It speaks to the importance of picking the right test for the right patient at the right time.”
Indeed, when it comes to a heart check-up, there isn’t a one-size-fits-all checklist. The most crucial factor is a frank conversation with your care provider. “There are a number of factors that go into choosing the appropriate tests,” explains Dr. Kuvin, who is the health system's Lorinda and Vincent de Roulet Professor of Medicine. “Everyone’s on their own path, and the clinician’s analysis can determine whether certain tests might be helpful.”
So what are the tests your doctor might recommend — and how can they help you stay healthy? Here are some examples, and what they can do for you:
Why you might need it: To get detailed information about your heart function, including the texture of the heart muscle.
How it works: You’ll lie on a platform that slides into an MRI machine. Often, dye is injected through an IV to help produce refined images.
What it shows: The size of the heart and its pumping power, damage or scarring from a previous heart attack or disease, heart valve function and other cardiac conditions.
Why you might need it: You need a baseline test or you have chest pain and shortness of breath.
How it works: While standing, you’ll be positioned between an X-ray machine and a plate that creates an image.
What it shows: “It provides a good view of the entire chest cavity and can give us information about the size of the heart and how it functions in relation to the lungs,” Dr. Kuvin says.
Why you might need it: You’re having new or worsening symptoms suggestive of heart disease or received abnormal test results that require further investigation.
How it works: A flexible tube called a catheter is inserted into an artery in your wrist or groin and threaded to the coronary arteries in your heart. Dye is injected to make it easier to get a detailed view of blood vessels on an X-ray image called an angiogram. You’ll likely get a light sedative to help you relax. As with Malin, results might lead to the immediate placement of a stent; a short hospital stay may be required.
What it shows: It can detect restricted blood flow to the heart.
Why you might need it: It can show whether there’s hardened plaque in the coronary arteries, which indicates a higher risk of heart attack.
How it works: You’ll lie on a table that slides into a CT scanner. Electrodes on your chest connect to a device that records heart activity and allows images of the coronary arteries to be taken between heartbeats.
What it shows: Levels of calcium-containing plaque in arteries that can restrict blood flow to your heart. Results can determine if you need medication or lifestyle changes to reduce your heart attack risk. (The test isn’t appropriate for someone with active heart symptoms, such as chest pain.)
Why you might need it: You have symptoms suggesting heart disease or received abnormal results from other heart tests.
How it works: You’ll lie on a table that slides into a CT scanner. An IV will inject contrast dye that will help blood vessels show up better on CT images. Chest electrodes will also record heart rate. You might require medication to slow your heartbeat so the images are clear.
What it shows: Detailed images of the arteries can detect abnormalities in blood flow, show areas of plaque buildup and pinpoint areas in need of treatment.
Why you might need it: You have symptoms such as shortness of breath, chest discomfort or palpitations; you had a heart attack; or you may have heart failure.
How it works: An ultrasound probe on your chest will bounce or “echo” sonogram waves off heart structures, showing moving images of heart walls and valves.
What it shows: “It’s a great window into the heart,” Dr. Kuvin says. “We can see how the heart is functioning, including the muscle, valves and surrounding tissue.”
Why you might need it: You need a baseline test or you’re having symptoms such as chest pain, shortness of breath, dizziness or palpitations.
How it works: Electrodes and wire leads will be placed on your chest, arms and legs. The leads are attached to an electrocardiograph machine that records your heart’s electrical activity.
What it shows: The electric impulses of the heart and whether you’re having abnormal heart rhythms; it can also reveal a history of heart attacks.
Why you might need it: You’re having symptoms while exercising, such as chest pain, shortness of breath or lightheadedness, or you want to make sure your heart can handle more rigorous exercise.
How it works: As you walk on a treadmill at varying speeds and inclines, an EKG will monitor the electrical activity in your heart. Your breathing, blood pressure and level of fatigue will also be tracked.
What it shows: It can help diagnose coronary or peripheral artery disease, determine heart attack risk and establish a safe level of exercise.
Why you might need it: If you’re experiencing new or worsening chest pain, shortness of breath or heart rate irregularities. It may also be recommended if an exercise tolerance test suggests you need more refined testing.
How it works: It’s just like getting an exercise stress test (see above), but you’ll also be injected with a radioactive tracer through an IV. This enables a nuclear camera to provide a view of the heart, how well it pumps and how blood flows. (Other kinds of stress tests use echocardiography or MRI to provide images.)
What it shows: It can determine specific areas of the heart that are not functioning normally.
Heart disease is the leading cause of death for men and women across the world. Seeing a cardiologist can make all the difference, but sometimes people don’t realize they should make an appointment, says Dr. Kuvin. ”We have advanced technologies that allow us to diagnose and treat heart conditions and improve and prolong life,” Dr. Kuvin says.
Here are some reasons to make an appointment with a cardiology provider:
Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.