Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.

It’s a number to make you sit up and pay attention: In 2020, Americans missed out on an estimated 9.4 million cancer screening tests, not to mention other routine care. Of course, postponing things like colonoscopies and mammograms seemed sensible at the time — Covid-19 precautions and pauses kept many from seeing their doctor for non-emergencies. But if you’re overdue for preventive care, now’s the time to break out your calendar and get those appointments on the books.
Need a little incentive? Take a look at the good news/bad news story told by cancer statistics. First the bad: Around 40% of us will develop the disease at some point, with cancer taking the lives of more than 600,000 Americans in 2020. And now the good news — more and more people are surviving. Between 1991 and 2019, the death rate dropped a whopping 32%. That means almost 3.5 million people survived cancer who may not have in previous years. One big reason for that remarkable improvement: Early detection.
Knowing your risk factors for disease is one of the first steps toward prevention and treatment. Then you and your primary care physician can work together to address health problems before they start. Examples of preventive care include vaccinations like the flu shot, yearly check-ups with your primary care doctor and other health screenings. Preventive care is important for successful treatment because:
Different patients need different health screenings at different ages. The guidelines for these screenings come from medical organizations such as the U.S. Preventive Services Task Force (USPSTF) and are based on the latest scientific evidence.
Finding cancer in its preliminary stages, before it has a chance to spread, can mean the difference between life and death. It also makes treatment easier, less invasive and less expensive. But many cancers are sneaky — growing for years before causing symptoms. That’s where routine screening comes in. These tests are designed to spot small abnormalities before they become bigger problems. Colon cancer is a good example: During a routine screening colonoscopy, doctors can spot and remove polyps or small growths that may, if left alone for years, turn malignant. Detecting cancer before it’s cancer? Talk about a win-win.
What it is
Two types of tests may help catch prostate cancer in its early stages. The first is a blood test called PSA, for prostate-specific antigen. A high level may indicate cancer. The other test is called DRE, for digital rectal examination. Here, your doctor inserts a gloved, lubricated finger into your rectum and feels your prostate for anything unusual. The DRE is less effective at finding prostate cancer than the PSA test, but it can sometimes be helpful.
How it helps
As with any cancer, early detection increases your odds of survival. When prostate cancer is caught early, almost 100% of men survive at least five years.
When to get it
The short answer: It’s complicated. The USPSTF recommends that men aged 55 to 69 with average risk talk to their doctor before undergoing prostate screening. There are several reasons, but a key one is that other common prostate problems can raise your PSA level, not just cancer. Plus, while prostate cancer can be deadly, most cases grow slowly or not at all — even if you have it, you may never experience symptoms. If you’re Black or have a family history of the disease, you’re at higher risk; your doctor is more likely to recommend screening.
Good to know
After skin cancer, prostate cancer is the most common cancer among men in the U.S. — one in eight men will be diagnosed with it.
What it is
A Pap test or Pap smear is the most common means of screening for cervical cancer. During a routine gynecological exam, your doctor collects a sample from the surface of your cervix, which is examined under a microscope for suspicious cells. A test for HPV (human papillomavirus) may be done on the same sample. HPV is a common virus that is the cause of many cervical cancer cases.
How it helps
It can take up to seven years for abnormal cervical cells to become cancer. If screening finds cells that have started on that journey, you’ll be monitored to see if they return to normal without any intervention at all, as often happens. If the changes are more substantial, you can have the abnormal cells removed before they turn cancerous.
When to get it
For most women between the ages of 21 and 65, the test is repeated every three years — more often if it finds abnormal cells. Alternatively, women 30 years and older can get an HPV test (or HPV test plus Pap smear) every five years.
Good to know
Cervical cancer used to be the deadliest form of cancer for women, but routine Pap tests made a dramatic difference. Now, cervical cancer doesn’t even crack the top five.
What it is
A mammogram is a set of four X-rays, with two views of each breast. To make the images, a technician presses your breasts one at a time between two flat plates. The compression may not be fun, but it’s over in seconds.
How it helps
Years before you have any symptoms, these images can reveal changes in your breasts that could become cancer. Finding breast cancer early lowers your odds of dying by 25% to 30%, possibly more. With early detection, you’re also less likely to need a mastectomy or chemotherapy, since a surgeon may be able to remove all cancer with a procedure known as a lumpectomy.
When to get it
If you’re aged 40 to 49, most experts recommend making the decision about getting a mammogram in consultation with your doctor, depending on your risk factors. Women between 50 and 74 who are at average risk of developing breast cancer should get a mammogram every one to two years. Over age 75, the benefits of the test decline — talk it over with your doctor. About to get a Covid booster? You may have heard that you should delay your mammogram for up to six weeks after the shot. But experts have looked at the issue and say it’s not necessary to postpone— so go ahead and get your test.
Good to know
Breast cancer is the second most commonly diagnosed cancer in American women. In 2022, experts expect it to account for around 30% of women’s cancer diagnoses. Your risk for breast cancer nearly doubles if your mother, sister or daughter has the disease — but even so, more than 85% of women who get breast cancer have no family history.
What it is
You have a couple of options here. The gold standard is a colonoscopy, in which a doctor examines your large intestine, colon and rectum with a special scope. During this exam, any suspicious tissue, called polyps, can be removed and examined in a lab. Colonoscopies require prep to clean out the colon and are typically done under sedation. For people with few risk factors, there are several other tests available. The simplest ones examine a sample of your stool for tiny amounts of blood. Another option, called sigmoidoscopy, is almost like a mini-colonoscopy: It’s done without sedation and takes less time, but it’s also less comprehensive.
How it helps
In the U.S., colorectal cancer is the second most deadly form of the disease — only lung cancer kills more people annually. But thanks to increased screening, the number of new cases has dropped every year since the mid-1980s. And diagnosing it early boosts your chances of beating it: More than 90%of people whose colorectal cancer is caught before it spreads survive at least five years after diagnosis.
When to get it
For most people, a first screening is warranted when you turn 45. You may need to start sooner if you have known risk factors: if you’re Black or have an inflammatory bowel disease, relevant family history or certain genetic syndromes. Over 75? Ask your doctor about screening.
Good to know
In 2021, the USPSTF lowered the age when screening should start from 50 to 45, because colon cancer incidence among people in their forties has been rising — jumping 2% every year from 2012 through 2016. Actor Chadwick Boseman was just 43 when he died of colorectal cancer.
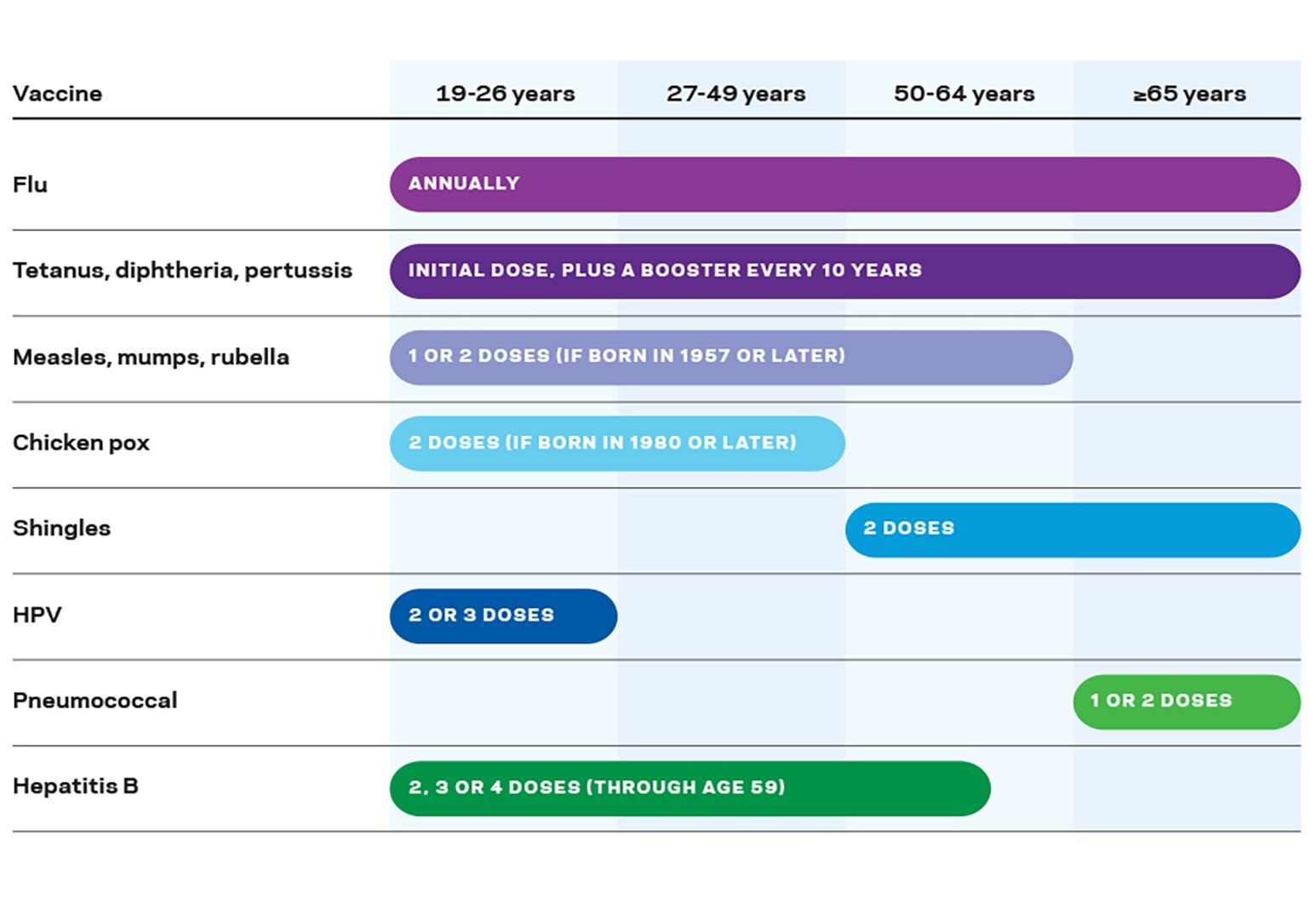
Screening tests can help flag certain diseases while they’re in the early stages, but vaccinations can help prevent some altogether (or, as we’ve seen with Covid-19 vaccines, ensure a milder case if you do get sick). Everyone should get the vaccines that follow, though their timing depends on age and risk factors — talk to your doctor about your individual needs. Other vaccines, like for hepatitis A, are recommended only for people with specific risk factors.
Having a regular check-in with your doctor ensures you’ll get several other routine screenings to monitor your health — or even save your life:
Experts recently added a must-do test that can protect your liver — and they recommend regular lung screening for select groups.
They call for checking adults aged 50 to 80 who either smoke now or quit within the last 15 years, and who have what’s known as a “20 pack-year” smoking history. That’s the number of packs you smoke a day multiplied by the number of years you’ve smoked. For instance, one pack a day for 20 years and two daily packs for 10 years both count as 20 pack-years. If you’re referred for screening, you’ll get a low-dose CT scan each year until 15 years after you quit.
Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.