Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.
Typically, respiratory syncytial virus (RSV) sends thousands of children to the hospital over fall and winter, peaking in January and February. But for the second year in a row cases have spiked early and continue to grow. This has led to unprecedented cases of the common respiratory virus across the U.S. On this episode of 20-Minute Health Talk, Cohen Children's Medical Center leaders Joshua Rocker, MD, and Margaret Duffy, PhD, RN, NEA-BC, discuss what they are seeing on the front lines in New York, the impact flu will have leading into the winter months, and how hospitals are responding to the need. They explain what parents need to know about RSV, and what steps they can take to reduce transmission within the home, particularly for those with children under the age of 1, who are at the greatest risk.
Meet our guests:
Find a pediatrician here.
Dr. Lindsay: 00:28
Hello, and welcome to 20-Minute Health Talk. I’m Sandra Lindsay. Today we speak with Dr. Josh Rocker and Dr. Margaret Duffy about the unprecedented surge of RSV cases hitting hospitals across the US as well as other winter viruses. Dr. Josh Rocker is Division Chief, Pediatric Emergency Medicine at Cohen Children’s Medical Center, and Dr. Duffy serves as the Chief Nursing Officer at Cohen Children’s Medical Center. Drs. Rocker and Duffy, welcome.
Dr. Rocker: 01:09
Thank you.
Dr. Duffy: 01:11
Thank you for having us today.
Dr. Lindsay: 01:13
In normal years, RSV sends thousands of children to the hospital over fall and winter. But for a second year in a row, cases have spiked early and leading to surges of the common respiratory virus across the US. So, Peg, typically RSV peaks in January and February. Why are we seeing this increase in the number of cases and hospitalizations now?
Dr. Duffy: 01:44
Sandra, that’s a great question. We’re not 100 percent sure what is causing this sudden surge in RSV, but most likely it is due to what happened during Covid. As everyone recalls, during Covid we all went into lockdown. Schools were closed. Children were sequestered at home. So many of those younger children, school-aged children, have had the past two years where they really have not had the exposure that children normally do during childhood to have the chance to catch and then develop immunity to various viruses.
As we emerged from the Covid pandemic and now we’re in an endemic phase, masks are coming off. We’re just so happy to have our socialization again, going to see our loved ones and our family, taking trips. Many of the transportation hubs are not requiring masks. So, basically, with masks off, we are seeing just a resurgence in it.
The other interesting feature, too, is that we seem to have lost some seasonality. We were seeing respiratory illnesses in July that we would normally see around the holidays. We believe that that’s what’s causing this along with the flu. So we’re going to make on behalf of Dr. Rocker and myself a shameless plug for that flu vaccine. Flu is very much we see in other areas of the world a conversion from moving out of RSV to flu, and we are seeing our fair share of flu illnesses as well, so get your flu vaccine.
Dr. Lindsay: 03:17
I’m also going to make a shameless plug for the Covid vaccine and the Covid boosters as well, Peg. So, thank you for that. Dr. Rocker, can you explain what our listeners should know about RSV?
Dr. Rocker: 03:33
RSV stands for respiratory syncytial virus. It is a virus we commonly see every fall, winter. For children above the age of 2, it generally cause a cold. Adults get it as well, and it causes a cold, congestion, runny nose, plus/minus fever. But in children under the age of 2, and more specifically under the age of 1, they get something called bronchiolitis, and bronchiolitis is different than bronchitis. Bronchitis is when you get mucus in the bronchi, and that’s when you’re coughing up loogies and green mucus. But bronchiolitis is lower down. It’s in the lungs.
So these children get fever oftentimes, cough, congestion, but then they get the wheezing. They have difficulty breathing as well. Not everyone, but it is frequent. Bronchiolitis is different than just a regular upper respiratory tract infection. It’s something that involves the lower respiratory tract as well. And these kids can get sick. So it’s very important for people to realize because there’s a lot of messaging in the news about RSV and then the hospitals — this is a completely different entity than Covid. RSV is extremely common. Yes, it is making kids sick, but RSV does not carry with it the same mortality or anything close to Covid.
Dr. Lindsay: 05:05
Those symptoms must be very scary for children and their parents.
Dr. Rocker: 05:13
One hundred percent. When someone is breathing hard, yes, that’s very nerve-racking to watch, and it’s challenging for the kids. The way I describe it is it looks like you’re running a race, but you’re not running a race. Your lungs are saying, "I need help getting air in." And the usual muscles that work to get the air in — it’s usually just the diaphragm up and down, but that work isn’t sufficient because there’s inflammation inside the lungs — so you have to recruit other muscles to help. If you’re doing that but there’s no reason for you to be exerting yourself, then that’s because the lungs are having difficulty or are a little bit too inflamed.
Dr. Lindsay: 05:57
How is RSV transmitted?
Dr. Rocker: 06:01
I think we learned a lot during Covid. I think we all became virologists and epidemiologists and learned how things got transmitted. RSV is not an airborne illness. There are respiratory droplets that kind of land on the ground, and then there’s contact transfer. RSV is transmitted mostly by contact transfer, but a little bit of respiratory droplet as well. But it’s basically it’s on the countertop, it’s on a toy, it’s on something. It’s on the doorknob. And children, the way they interact with the world, they love to touch things. They love to touch things and they love to put things in their mouth. So if you’re in daycare or if your older sibling is in daycare and gets RSV and then comes home and they’re sneezing and touching things, that’s how the child is going to get it as well.
Dr. Duffy: 07:00
Sandra, that’s a really good message to the folks who are listening today in terms of minimizing the potential spread of RSV and respiratory viruses. Hygiene practices are so important. We do a lot of education with parents and caregivers around hand hygiene. What we all learned in kindergarten, washing your hands is so important. So making sure when you’re children come home from school or they come home from the playground or when they’re out with their friends, making sure that they are washing their hands. Not touching their face and minimizing that, and if that happens, then doing simple hand hygiene.
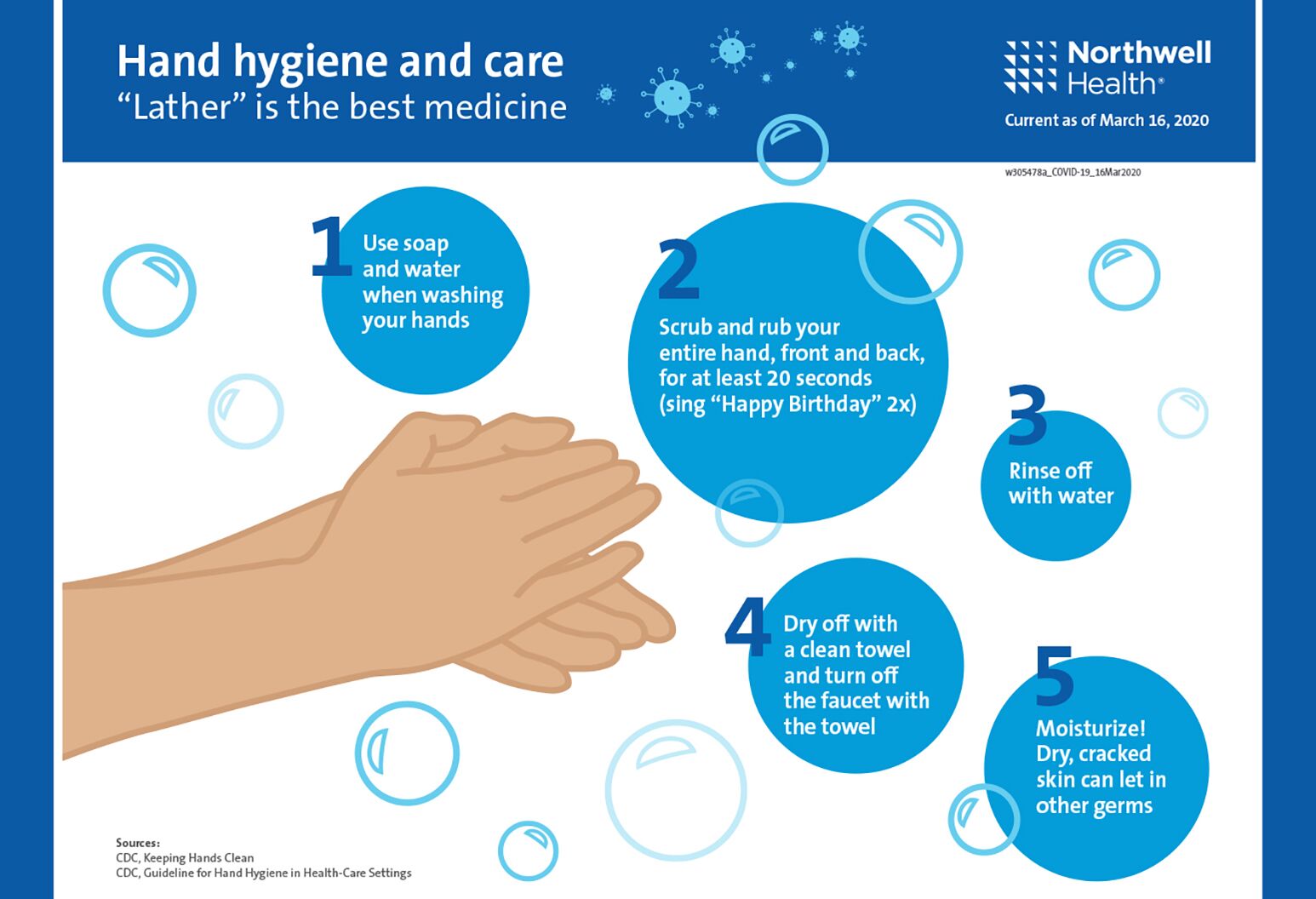
A 5-step plan for clean hands
We all get concerned here at the hospital as we go into holiday season. We’re looking forward to spending our time with our friends and family. There’s so much burnout from COVID that you really want to have those warm family gatherings as we look forward to Thanksgiving and then the December holidays. But we really encourage families, particularly those with the very young infants under 2 months of age, to really think about who is being exposed. So the very young and very old, the opposite ends of the spectrum are those individuals at risk. As much as we want to be together, I think the message is to try to be smart and to protect particularly those young, young infants.
Dr. Lindsay: 08:20
It also sounds like it would be beneficial to just have a routine of wiping down our surfaces as well.
Dr. Rocker: 08:29
I think that definitely makes sense. One thing about the hand hygiene that we talked about, we say washing hands, but the important — because I think a lot of times, people put the soap in the palm of their hand, rubs their palms together and then wash it off, but it’s the fingers that come to our noses, come to our mouth, come to our eyes. So it’s actually washing the fingers that are the most important part of the hands.
Dr. Lindsay: 08:51
What are some supportive kind of therapies that you’re using?
Dr. Rocker: 08:57
That’s a term that’s used a lot. We don’t have any treatments, but we can give you supportive care, and I just want to clarify what that means. So treatments stop the virus, kill the virus. We don’t have that. But supportive care is if your oxygen is low, I’ll give you oxygen. If you’re dehydrated, I’ll give you fluids. If your lungs are working so hard, I can put you on machines that make breathing easier for you. We support you and your body until the virus goes away and you recover. So if there’s really poor feeding, difficulty breathing, we definitely want to see those children. But if it’s fever and otherwise they seem to be doing well, that’s certainly something that you can follow up with your pediatrician, but there’s not necessarily the urgency to come to the emergency department unless you’re below a certain age. If you’re below 2 months and you have a fever, we do want to see you in the emergency department.
Dr. Lindsay: 09:58
How do you make the diagnosis?
Dr. Rocker: 10:02
The diagnosis of RSV, specifically RSV, is a respiratory viral swab that we do, and then it’ll tell us if it’s RSV. However, I don’t want the audience to think that RSV is the only virus that causes bronchiolitis. Bronchiolitis can be caused by a bunch of other viruses, but right now, the large majority of the children that we’re seeing with bronchiolitis are in fact RSV.
Dr. Lindsay: 10:30
Awesome. So who is most at risk for a severe RSV?
Dr. Rocker: 10:36
That’s a great question. Those who are most at risk as we mentioned were those under the age of 1, specifically even younger, and then premature babies as well are at higher risk. We are seeing some older kids who may have complex medical conditions who are a little bit more fragile and when they get RSV, it may be more challenging for them, but it’s really the younger kids that we’re most concerned about.
Dr. Lindsay: 11:06
As an adult, should I be concerned about RSV?
Dr. Rocker: 11:12
Generally, no, but as an adult who has children or who has children who have children, that’s something that you should be a little bit thoughtful of. I just want to stress one thing. We’re busy. We have never seen higher numbers in our emergency department ever, and I’m saying by 50 percent more than extremely busy times. In regards to the public health message to the adult, it’s be thoughtful about the children because we’re in a crisis right now.
Dr. Lindsay: 11:52
When did we really start to see RSV hit this year?
Dr. Rocker: 11:58
I would say probably four weeks ago it was trickling in, and then three weeks, it really started taking off. December is kind of when traditionally flu comes in a little bit more with a vengeance. We’re expecting even higher numbers then. So RSV tends to be a little bit of a hump, not a big spike, so we anticipate RSV to still be around well into December and parts of January, and we know it’s going to be overlapping with flu at that point as well.
Dr. Lindsay: 12: 29
Dr. Rocker, do you think the higher number of infections you’re seeing will be a one-time event or a new normal? Is the pattern of the virus changing?
Dr. Rocker: 12:41
We’re not certain. We know, as Peg mentioned, last year was different than this year. This year is a little bit closer to normal but definitely abnormal. And I think we suspect that it will trend back to the old ways just because the logic with COVID is that we weren’t socializing, and now we are socializing. COVID didn’t change viruses. I suspect, strongly suspect, that next year barring any other social, bizarre phenomenon that we’ll probably be back on par.
Dr. Lindsay: 13:21
Peg and Dr. Rocker, have you seen anything like this in your practice before?
Dr. Duffy: 13:28
No, not at all. We’ve gone through H1N1, we’re gone through other types of infectious processes, but to have so many children particularly concentrated at the very young to become so acutely ill at almost the same time, and sometimes we describe it as a tsunami and it comes in waves. We might have maybe 12 hours where the volume is a little bit less which actually we take a breath and we say well, that 12-hour volume not’s so bad. That would have been a busy day two years ago, right? So everything is relative. But to be honest, no, this is something, and I’ve been practicing for decades, it’s been unprecedented.
Dr. Rocker: 14:16
I remember when we set up flu pods in the 2018-2019 flu season and that was really much more an outpatient burden where we had so many patients coming in who are concerned and they generally were fine. And the same with H1N1. The atrium of the Children’s Hospital basically became a testing center and an urgi (PH) center. But it didn’t impact the admissions nearly as much as this is right now. To Peg’s point, I have never seen us borrow space from the adult side, and we desperately needed it when we received it. It’s a different entity than we’ve seen in the past.
Dr. Lindsay: 15:04
Can you talk to us a little bit about your strategies to manage the volume?
Dr. Duffy: 15:10
Last year, we did quite a bit of planning, predicting almost what you can’t predict. But seeing that we had lost some seasonality, as a leadership team, we came together and said how can we — if this comes and in a wave that may be unexpected, how can we be ready for it?
So we had hired up. We looked at all of our alternative spaces. We looked at our surge plans and said how can we become more flexible and nimble? So what we’ve ended up doing is having a lot of satellite spaces. We’ve borrowed a unit from our Long Island Jewish friends. They’ve been very gracious. We’ve repurposed areas here within Cohen’s for the emergency department. We’ve had to staff up. We’ve been doing this for months now, so that we are positioning ourselves to provide that quality care that we are known for. But it’s been challenging. It’s been very challenging. As we see the acuity, the severity of illness go up, it is a challenging concern.
Dr. Lindsay: 16:15
Dr. Rocker, what role does COVID and influenza play in this RSV surge?
Dr. Rocker: 16:24
COVID hasn’t left us. It is a smoldering virus that is there, and we still have patients who are admitted with COVID. It is certainly not overwhelming our numbers, but it’s a presence, and influenza currently is on the rise. We definitely are seeing it in some patients. I expect it to be a much more significant thing in the weeks to come.
Dr. Lindsay: 16:50
Dr. Rocker, what can parents do to keep their children out of the hospital, to prevent their kids from getting RSV?
Dr. Rocker: 17:01
With kids going to school, it’s hard to prevent RSV transmitting in the community. We’re happy that kids are in school. We’re happy that kids are without masks, and we’re happy that they’re developing normally in an appropriate environment. It’s not just kids. It’s specifically the young kids, right? The ones that are being hospitalized are the ones that are the newborns, under 1 year of age, so be more cautious with those kids. And for those siblings in a household who have a child who is less than 1 year of age, they may have a common cold. They may come in with a runny nose, congestion. Maybe that’s where you should do a little distancing in the house, wash the counters a little bit more.
Dr. Lindsay: 17:54
I couldn’t end this podcast without asking how are you and the team coping with this surge?
Dr. Duffy: 18:01
One thing that we do well here is really support each other. We have an incredible support system on each unit. They really are a family here. I’m really proud. We’ve had people who’ve come here for short stints and they decide to work here because the team is just so really incredible. We have holistic nurses who help support our team members on the frontlines through Reiki sessions. They go to the units. We have a system called Team Lavender where we’ve got specially trained individuals who will go to the units to help support, particularly if there’s a really challenging case, an ethical issue, a death of a child, to really support that team through that event whether it’s in the emergency department or on the inpatient units. Our chaplains here are just really incredible. So there’s lots of communication among our team both at the senior level as well as throughout our leadership level down to our frontline team members throughout all of our disciplines.
Dr. Rocker: 19:10
I’d like to just reiterate what she’s saying. I think the heart in this institution is big, and it’s big because we’re caring for vulnerable children. But it’s big because people just like working with whom they work with. So I just completely agree with what Peg is saying. There’s a lot of camaraderie. After shifts, there’s a lot of oh, my gosh feelings, and there’s lots of text messages and sharing of stories, and that’s what gets you through the day. It’s the relationship, it’s the camaraderie, and it’s the knowing that the team has your back, and I think our team feels that way.
Dr. Lindsay: 19:51
I felt that camaraderie and teamwork, and it was so palpable when I visited and toured some of the units with Peg. Absolutely. Drs. Rocker and Duffy, thank you so much for joining us on 20-Minute Health Talk. And to you the listener, thanks for tuning in. I’m Sandra Lindsay. Have a great day and be safe.
Hear Northwell experts break down the latest news and developments in this new podcast.
Our representatives are available to schedule your appointment Monday through Friday from 9am to 5pm.
For a Northwell ambulance, call
(833) 259-2367.